
PHISICC
Co-creating tools for health workers to support decision making, increase their dignity and improve health outcomes
Approach
PHISICC is a paper-based clinical support and data collection innovation which grew out of a collaboration between health workers and health ministry officials from Côte d’Ivoire, Mozambique and Nigeria with public health experts, doctors, and designers.
PHISICC uses the transformational power of design to reframe the role of health workers in remote, rural areas from basic service functionaries to active partners in the health of their patients.
By providing health workers with tools that centre their own diagnostic and decision making intelligence over the rote documentation of health data, PHISICC has had a significant, rigorously tested impact on health outcomes while privileging health workers’ experience.
The Challenge
In many Sub-Saharan African countries, more than 60% of the population live in rural areas. Health facilities in these locations are typically isolated, under-equipped and managed by one or two staff with only basic healthcare training.
Working under difficult conditions and charged with diagnosing and treating a full range of both chronic and acute diseases, health workers in many African countries are also under enormous pressure to document and report data on health indicators to centralised health ministries and the international donors that fund them.

While the data collected by health workers is critical to informing health policy, international funding decisions, and the eradication of preventable disease, the old fashioned ledgers used to collect this data have been produced and reproduced for years with minimal-to-no attention given to interaction design. It is typical for the health workers we worked with to spend two to three days out of every month reporting on their activities using these cumbersome paper registers.
The broadly accepted response to the improvement of this situation is to propose digital infrastructure and applications. But in a context where only 9% of rural areas have stable electricity, limited-to-no cellular network coverage, and chronic underinvestment in infrastructure of all types, paper-based solutions are a cost effective, pragmatic approach
“We have moved from nursing to medical care. [PHISICC] allows us to really have quality diagnoses, reliable data that allow us to be able to treat our patients and do the treatments like a doctor… We have become equal to doctors.”
Health Worker in Côte d’Ivoire
Outcomes
PHISICC offers a set of clear, elegant decision making tools covering the full range of common medical conditions which centres the experience of health workers and their patients while still meeting the data collection needs of health ministries and donor agencies.
PHISICC is a design system composed of:
- Visual cues differentiated by clear information hierarchy
- Sequential processes following clinical best practices
- Immediately legible iconography
Through a series of visual questions, the PHISICC tools foster informed, diagnostic conversations between health workers and patients. They make the algorithmic logic of the very best clinical practices intuitively available to even minimally trained health workers. Checking boxes and noting observations with PHISICC both improves the quality of clinical decisions
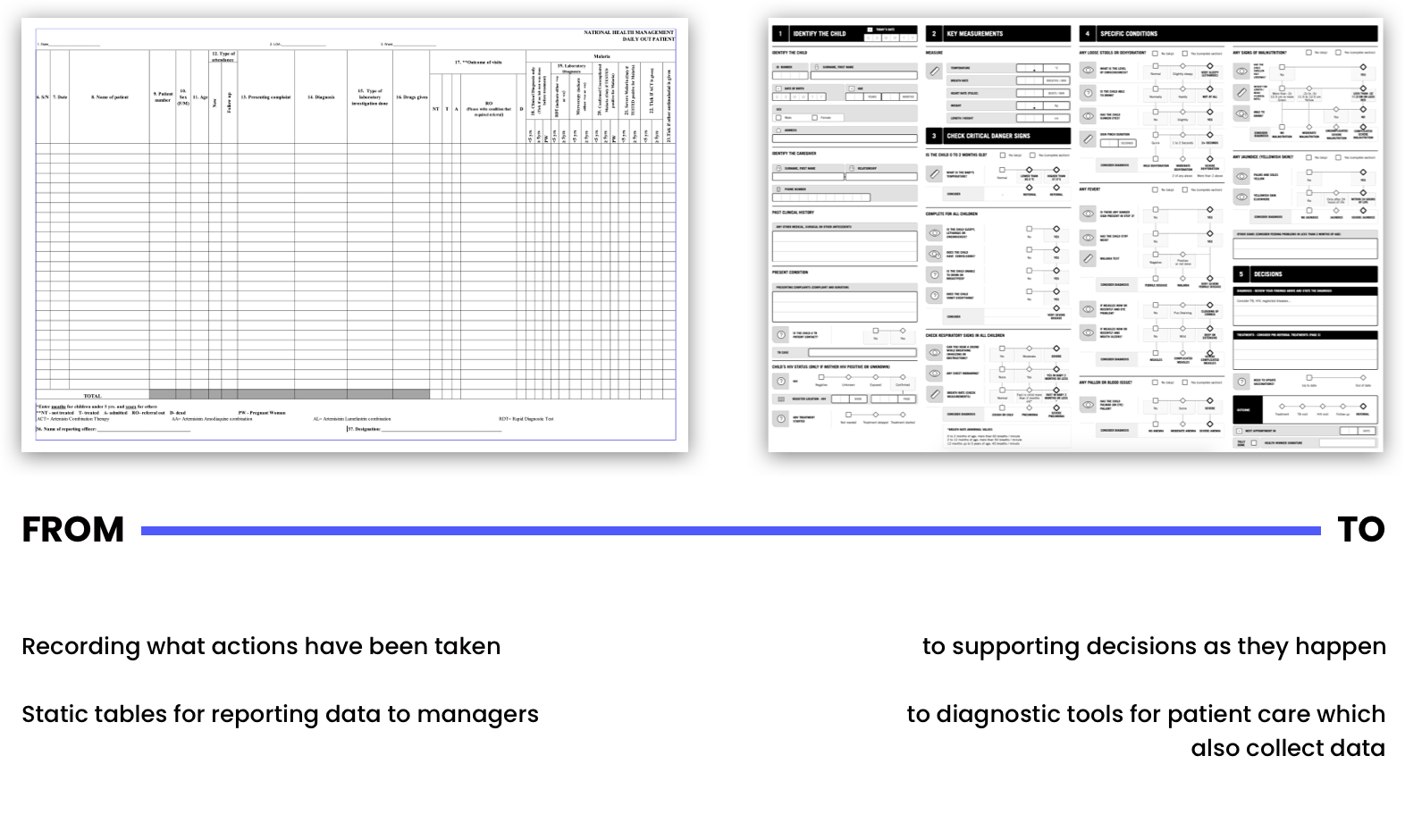
Old VS New design
Comprehensive and Cost Effective
Many attempts to pilot innovations in rural health have taken place, and the PHISICC tools solve for many of their limits, by
- covering a full range of primary care topics: antenatal care, child delivery, postnatal care, vaccination, sick child, outpatient consultations, HIV and tuberculosis and serve as a critical tool for collecting the data which informs national healthcare policy.
- being locally produced and designed to be low cost and simple: A4/A3 paper, high contrast in black and white, to allow for reproduction by health workers via photocopying if necessary.
- using simple visual hierarchy for the sequential tasks during a clinical interaction
- presenting clear iconography to guide clinical actions: observe, measure, question
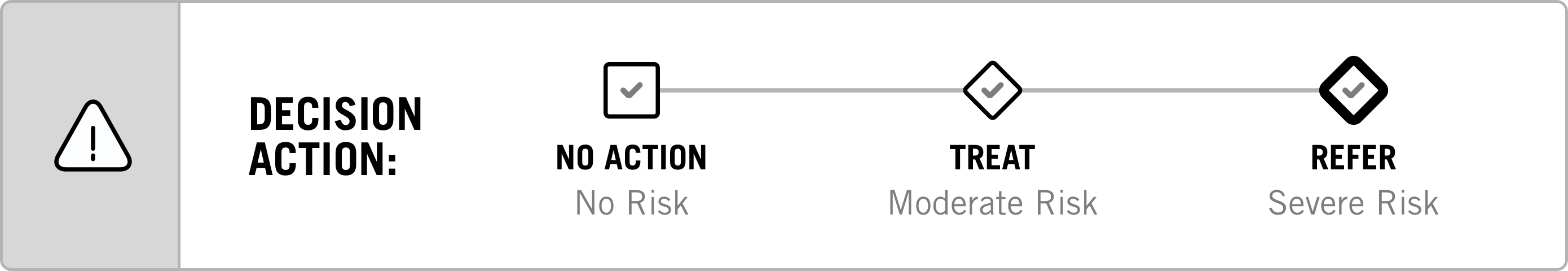
- including algorithmic decision pathways: assess, diagnose, treat, refer
- supporting decisions which prompt discussion about follow-up visits/actions
- Below there is an overview of different components of the health information system, including the decision making visual language, components of the health outcomes and a page of the Sick Child Register.


The Impact
The impact of a design intervention is rarely studied using rigorous, scientific methods, but if design aspires to create social impact and be considered an equal partner alongside primary players in fields like public health, its effects need to be measured using the same standards applied to other health interventions; which is why once designed, PHISICC’s impact was measured using the most rigorous scientific testing standard: a randomized control trial. This took place
- in 210 health facilities, covering more than 4 million people
- in 3 countries
- Over 1 year
The health facilities were organized into two groups: one using PHISICC and the other continuing to use the routine system, during one year. The PHISICC tools had the following impact:
- Mothers’ overall satisfaction increased (Nigeria)
- In mothers using health services, there was an increase in all overall satisfaction and in 4 of the specific satisfaction parameters (Nigeria)
- Health workers felt better valued by their superiors, with a score that increased by more than 10%(Mozambique)
- Health workers claimed they were more valued by their superiors (Mozambique)
Key results:
12%
increase of children receiving vaccines for preventable disease (Côte d'Ivoire)
25%
more children were diagnosed and treated properly (Nigeria)
50%
reduction in over-prescription of medication for sick children (Côte d'Ivoire)
4.4h
saved when doing the monthly reporting (Côte d'Ivoire)
10%
health workers felt better valued by their superiors, with a score that increased by more than 10%(Mozambique)
Other projects

OpenMRS 3.x
Redesigning an open-source electronic medical record system used in low-resource settings around the world
Kenya
Uganda
Haiti
South Sudan

VxData Insights
Exploring why immunization workers underutilize data in their decision-making
Kenya
Mozambique
Congo [DRC]





